23 Feb The Future of General Practice
It is time to reflect on the future of health care. A new federal health minister notwithstanding, there have already been massive shifts in key areas of service delivery, and we can expect more to come. There are three areas that I believe will impact the way general practice functions in the future, which we must understand if we are to successfully ride the coming wave of change.
1. Systems
No matter what angle you look at it from, the health system is complex. The interplay between departments, jurisdictions, and funding arrangements means it is extremely difficult to effect meaningful significant change. Throw in the multitude of social determinants, with their own impacts on health outcomes, and the picture takes on a distinctly Byzantine character.
“no matter how much we may wish to operate independently of systems, our realities are undeniably bound up in them”
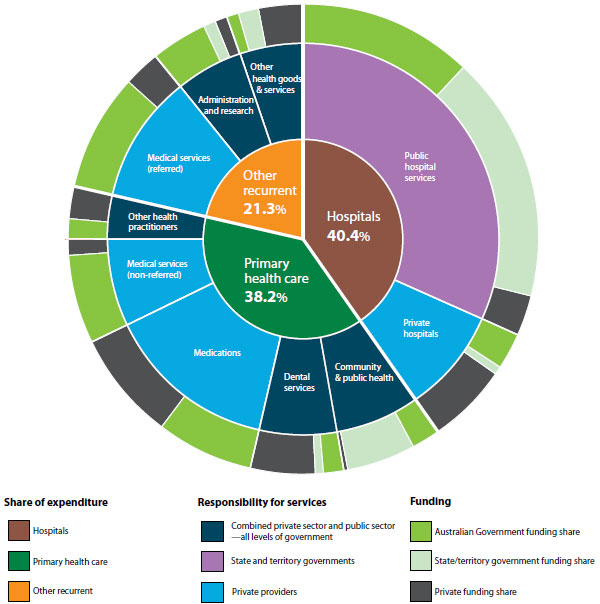
Source: Australian Institute of Health and Welfare
As GPs, no matter how much we may wish to operate independently of systems, our realities are undeniably bound up in them, and changes to one part of a system frequently have unforeseen consequences. Nowhere is this more clearly seen than in the case of changes to Medicare item numbers, which led to not just an increase in after hours billing, but entirely new corporatised medicine business models adopted in order to maximise billings.
What does this mean for the future? The first phase of Health Care Homes has been commenced in 10 primary health networks across Australia. This model will see payments to practices shift from a fee-for-service model towards capitation and outcomes-based funding. Whilst this may sound good in theory, there is much discussion to be had about levels of funding and measuring outcomes before there is any chance of broad acceptance within the medical profession. If we accept that there are systemic drivers within a fee-for-service system to provide more services to patients, then the reverse situation should apply under capitation. This means that the system incentivises the doctor to NOT see the patient. Studies looking at the behaviour of physicians under different funding models confirm this broadly, but lack the quality and Australian data required for certainty.
2. The Profession
Evidence-based medicine has not always been the norm, having emerged from a slow paradigm shift in the decision making tools and attitudes of medical professionals. From the time of Hippocrates to about 50 years ago it can be argued that decisions about medical care were in fact “eminence-based”. Physicians imparting their wisdom from experience and anecdote were the norm, held in high esteem and rarely questioned. The emergence of the randomized controlled trial was a huge leap forward, but access to information remained a limiting factor in effective decision making until the coming of the information age, and the internet. This increased access to information has its own set of risks and rewards, which are evident to anyone who works in health care.
“Health care is increasingly being delivered in a partnership arrangement rather than from a pedestal.”
The primary enabler of increasing patients’ rights and autonomy has been access to information that was once completely in the ownership of the doctor. This has allowed concepts such as team based care; patient centred health care and shared agendas to flourish. Health care is increasingly being delivered in a partnership arrangement rather than from a pedestal. This enormous shift in the balance of power in the patient-doctor relationship is now the largely accepted n within the profession and the community.
3. Emerging technologies
Technology has revolutionised our lives in the space of a generation, and medicine is following suit. Advances in the understanding of genetics have allowed the development of highly individualized risk assessments and treatment plans. Nanotechnology and 3D printing bring the promise of distribution of health solutions to practices and consumers. Mobile technology and wearables can now be used to monitor a whole range of health data, for storage on devices or uploading and sharing with health care providers. The emergence of patient controlled electronic health records and telemedicine provide additional tools to support the shift in control and responsibility for clinical data to the patient.
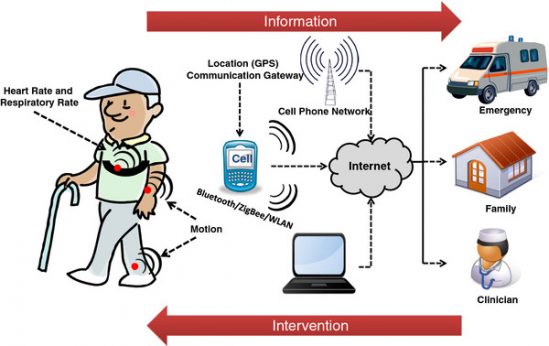
Through new technologies such as wearable devices, patients are having responsibility for clinical data shifted their way.
Source: https://jneuroengrehab.biomedcentral.com/articles/10.1186/1743-0003-9-21
What does all of this mean for the future of general practice?
We have a health care system that is increasingly incentivised to keep patients at home. We have had a paradigm shift in the dynamics of the relationship between doctors and patients, with the patient more likely to take the lead role in decision-making. We now have the technologies that empower the patient to collect and use data with remote input from the clinician.
The days of the doctor and the doctor’s office being the central point in patient care are coming to a close. Will we embrace the change or rail against it? Whatever we think, change is coming; there is nothing more certain.